The ankle brachial index is a medical test used to help identify peripheral artery disease (PAD).
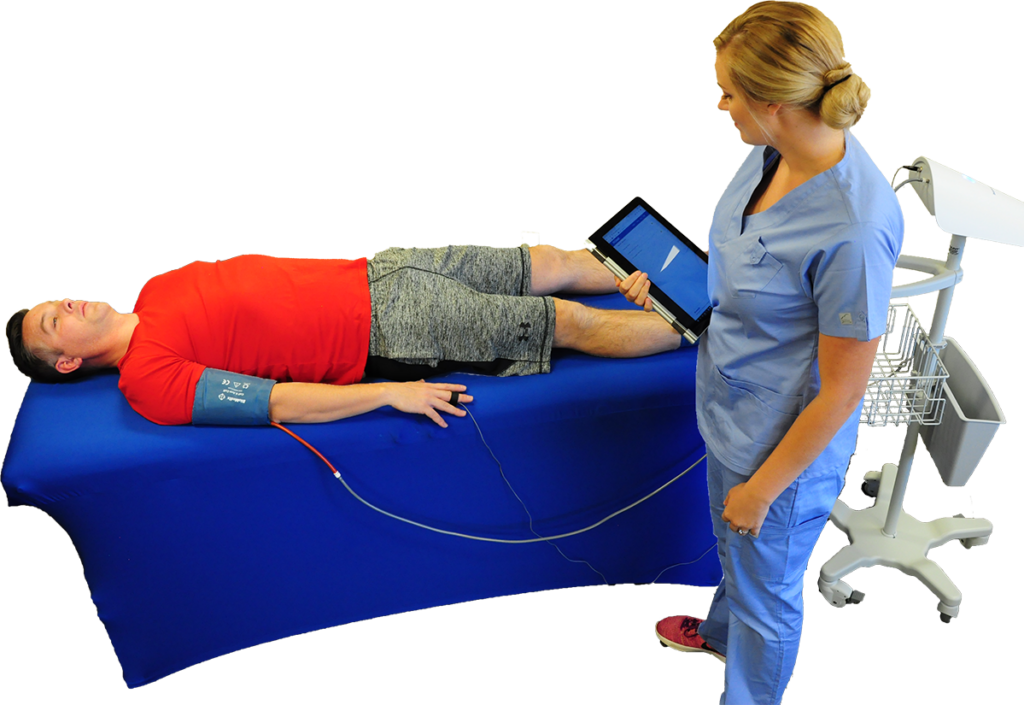
PADnet® is a quick and easy way to perform an ABI test, and can typically be performed by a medical assistant, and be evaluated remotely by a vascular specialist.
What is an ankle brachial test?
An ankle brachial index test consists of the blood pressure measurement of a patient at the arms, and then comparing them with the systolic blood pressure at each ankle. Typically, a blood pressure cuff is are used to occlude flow to the artery, and sometimes oscillometry is used to calculate the systolic pressure (oscillometric ABI), and sometimes other sensing technologies, like doppler, are used to determine when blood flow has returned to the artery.
Why is the ABI important?
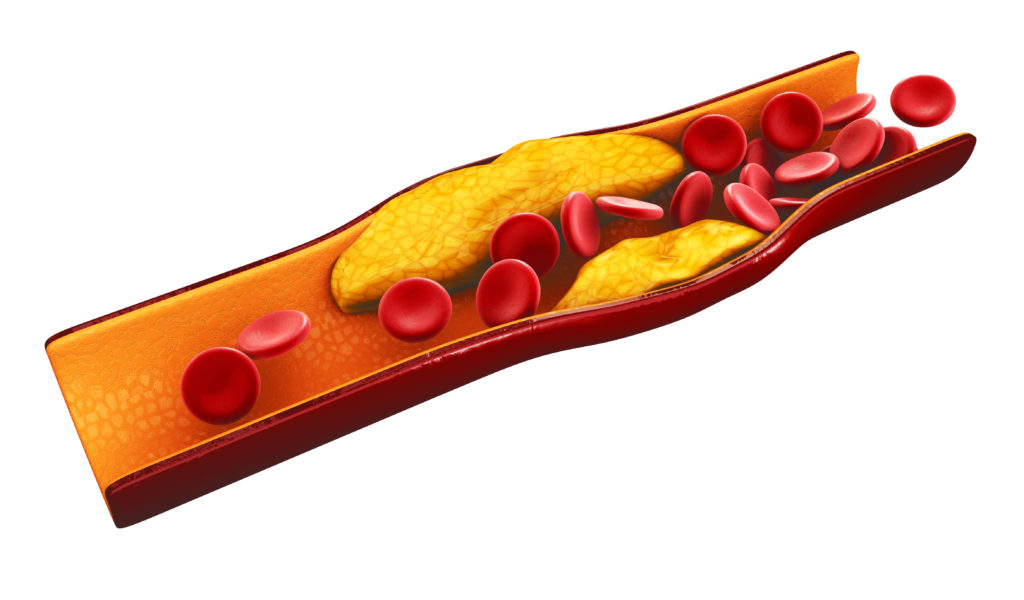
The ABI is an important measure of the blood flow to the lower extremities. This testing is an important way to assess cardiovascular health because atherosclerosis (arterial plaque buildup) can sometimes occur in the arteries delivering oxygen-rich blood to the legs and feet.
If a patient has diabetes, assessing blood flow through physiologic testing like an ABI, is critical for care management. For example, a patient with diabetes and PAD may qualify for diabetic shoes to prevent slow-healing ulcers from developing.

What does a patient’s ABI index mean?
If the blood pressure at the arm is less than the blood pressure at the ankle, it can mean that blood flow is compromised, oftentimes due to arterial plaque that has developed in an artery closer to the heart.
The ABI is just one measure used to help check for PAD. Pulse volume recordings (PVRs) is another clinical data point, and a patient with an abnormal ankle brachial index test or abnormal PVRs may need to confirm a PAD diagnosis with duplex ultrasound imaging.
Typically a resting ABI between 1.0 – 1.4 is considered to to be a normal ABI, while an ABI value below 1.0 could indicate narrowed arteries in the blood vessels of your lower extremities.
The chart below is based on what the ACC/AHA (American College of Cardiology and American Heart Association) says about the ABI. If a patient have a low ABI, a healthcare provider may refer them to a vascular specialist.
ABI 1.00 - 1.4
Normal*
ABI 0.99 - 0.91
Boderline
ABI 0.90 - 0.51
Mild - Moderate
0.5 or less
Severe
* This information is intended for informational purposes only, and should not be construed as medical advice.
How do I calculate an ABI index?
After getting systolic blood pressure, you divide the highest of the arm pressures by the ankle pressure for each side to get the ABI for each side of the body. In addition, you should have a specialist (like a doctor who performs vascular surgery)interpret your ABI study for validation.
Also, if a patient’s ABI test is over 1.4, or you are having trouble getting a blood pressure due to non-compressible ankle arteries, especially with diabetic patients, you may need to consider other diagnostic data to evaluate. For example, patients with diabetes will sometimes also get a TBI test, which evaluates blood pressure at the toes rather than the ankles.
Sounds complicated? See below for a solution that greatly simplifies the process.

ABI Testing For Your Practice
PADnet is the only diagnostic device on the market that can support the identification of peripheral artery disease and venous reflux disease through a unique collaborative care model.
Patients with PAD are six times more likely to die from cardiovascular disease (like coronary artery disease, or CAD)than those without PAD. However, PAD is an under-diagnosed disease, and patients oftentimes do not get proper care until the associated heart disease becomes evident.

Who can perform an ABI test?
With PADnet, all of our ABI systems come with studio training. If you have a medical assistant that can use blood pressure cuffs to get a systolic blood pressure, they can perform a PADnet test.
Performing an ABI test used to only be possible in vascular laboratory settings, but with technology like PADnet, healthcare professionals in a variety of primary care settings, such as community health clinics.

Have there been a systematic review of the ankle-brachial index test?
Studies have stated, “To date, the ABI is the most effective, accurate, and practical method of PAD detection. A diagnosis of PAD is based on the presence of limb symptoms or an ABI measurement less than 0.9”. Other studies have commented on the use of the ABI combined with Pulse Volume Recordings (PVRs), saying, “PVR waveforms and segmental pressures are complimentary tests.”
In terms of accuracy, the Trans-Atlantic Inter-Society Consensus Document for the Management of Peripheral Arterial Disease (TASC II) found, “Segmental Leg Blood Pressure and Pulse Volume Recording measurements alone are 85% accurate compared with angiography in detecting and localizing significant occlusive lesions. Furthermore when used together, the accuracy approached 95%.”
Is there an Ankle Brachial Index CPT code?
Some sources indicate that an ABI test is part of the physical examination and is not reimbursable.
With PADnet , you can generate other diagnostic data, such as PVRs, which qualify the study to be reimbursable as a noninvasive lower extremity study for CPT codes 93922 and 93923. In addition, you can perform post-exercise ABI studies for CPT code 93924.
For traditional fee-for-service healthcare providers, typically payors require that a patient present with symptoms of PAD, like claudication (leg pain while walking) or resting leg pain to get reimbursed.
Why is the ABI important?
The early detection of atherosclerosis in the lower extremities can help with patient risk stratification in regards to other cardiovascular diseases. Studies have found that 75% of patients with PAD also have heart disease. Other studies have found that 40% of patients with PAD also have CHD as well as cerebrovascular vascular disease.
The importance of the early detection of PAD is critical to improving patient outcomes, because studies have shown that 30% of those with PAD are likely to die from a stroke or heart attack within 5 years.
I’m not a healthcare provider, but I’m worried I may have vascular disease, what should I do?
If your legs hurt when you walk, and especially if you have cardiovascular risk factors such a high blood pressure, make sure to talk to your doctor, and ask about getting a test to see if you have peripheral vascular disease. Lifestyle choices such as unhealthy eating, lack of exercise, and tobacco use all increase your risk from PAD too, so it’s important to start making healthy choices today.