Typically, providers are only reimbursed for PADnet® testing in patients presenting with primary indications, or symptoms of Peripheral Artery Disease (PAD). Biomedix can help with a variety of ways to help providers identify patients with PAD symptoms, including:
- Surveys to help patients self-identify PAD symptoms
- Training to identify physical clues of circulatory issues in the lower extremities
- Analyzing patient charts in practice EMRs to identify patients already reporting PAD symptoms
- Identifying patients in at-risk populations for PAD for targeted consultations regarding potential symptoms which may go unreported
- Educational PAD posters
- Tri-fold PAD brochures for waiting rooms

Asymptomatic PAD
Studies have shown that only 5% of people with PAD present with the classic primary indication of intermittent claudication, while 30% present with atypical symptoms (e.g. pain not present in the calves, pain that doesn’t subside after 10 minutes of rest, or pain that doesn’t stop a person from walking), and 65% do not complain of symptoms at all[i].
In addition, in patient populations with comorbidities that impact mobility, such as arthritis, cardiac disease, and pulmonary disease, the lack of exercise or exertion may result in patients not reporting claudication, or the pain being attributed to the comorbid disease[ii].

PAD Symptom - Intermittent Claudication
Intermittent claudication is typically the first classic symptom of PAD. Intermittent claudication is defined as leg discomfort while walking that improves at rest, and typically manifests itself in patients it impacts as a consistent throbbing soreness in the calves, thighs, buttocks, hips or feet. The cause of this discomfort is typically the result of insufficient blood flow to the lower extremities causing a lack of oxygen to the muscles required for walking and exercise.
Although the discomfort experienced with intermittent claudication is typically cramp-like uneasiness, it can sometimes be experienced as fatigue, weariness, numbness or tingling, causing PAD symptoms to be misidentified by a health care provider.
It’s important to note that since the pathophysiology of atherosclerosis is slow and progressive because plaque builds up in the arteries over time, a patient experiencing intermittent claudication may have had PAD for a long period of time before reporting symptoms to a health care provider.
In addition, studies indicate that only 20% – 30% of PAD patients may present with symptoms, possibly because PAD patients are avoiding exercise to avoid pain[iii]. Other studies have found that whether or not a patient with PAD is presenting with typical symptoms does not have an impact on PAD-related mortality[iv].
The ICD-10 codes for claudication are:
- I70.211 (right leg)
- I70.212 (left leg)
- I70.213 (bilateral)
- I70.218 (other)

PAD Symptom - Ischemic Rest Pain and Critical Limb Ischemia
When PAD progresses, typically the discomfort of intermittent claudication becomes more severe, and takes less exertion to trigger the discomfort. As blood flow continues to be further constricted, patients will begin to experience lower extremity discomfort at rest. This discomfort is typically experienced in the feet first, and often at night, because leg elevation decreases blood flow.
When a patient is experiencing leg discomfort at rest related to PAD, the patient is considered to have an advanced form of PAD called critical limb ischemia (CLI)[v] which can progress to critical limb threatening ischemia (CLTI).
The ICD-10 codes for resting leg pain are:
- I70.221 (right leg)
- I70.222 (left leg)
- I70.223 (bilateral)
- I70.228 (other)

PAD Symptom - Ulceration, Gangrene and Amputation
The body needs oxygenated blood flowing to the extremities to ensure proper tissue viability and enabling the proper recovery from cuts, blisters, or other minor wounds. If lower extremity blood flow is compromised, a wound on that extremity will typically be slow to heal, increasing the risk of infection.
The ICD-10 codes for ulcerations are:
- I70.231 (right thigh ulceration)
- I70.232 (right calf ulceration)
- I70.233 (right ankle ulceration)
- I70.234 (right heel/ midfoot ulceration)
- I70.235 (right other part of foot ulceration)
- I70.238 (other part of lower right leg ulceration)
- I70.231 (left thigh ulceration)
- I70.232 (left calf ulceration)
- I70.233 (left ankle ulceration)
- I70.234 (left heel/ midfoot ulceration)
- I70.235 (left other part of foot ulceration)
- I70.238 (other part of lower left leg ulceration)
If a wound that is infected isn’t properly treated, the infection causes localized death and decomposition of tissue at the wound site, typically referred to as gangrene. A wound that has progressed to gangrene typically requires amputation to stop the progression of gangrene to other parts of the body.

Lower Extremity Review (LER) magazine publishes an update on Peripheral Artery Disease (PAD)
PAD & Intermittent Claudication
Duke University Health study: use of diagnosis codes to identify PAD in EHR claims
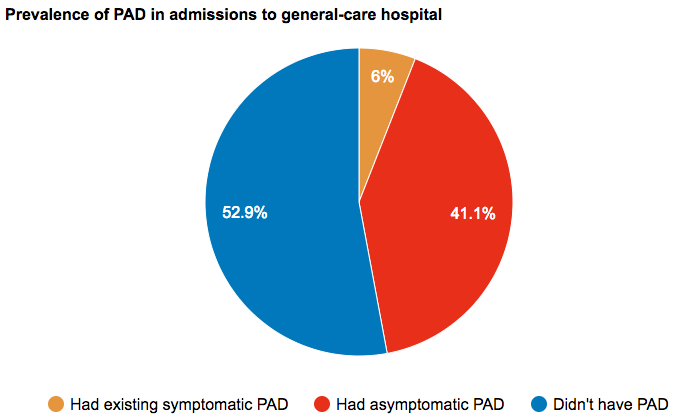
How frequently is PAD asymptomatic? A study from admissions to a general hospital.
[i] McDermott MM, Applegate WB, Bonds DE, Buford TW, Church T, Espeland MA, Gill TM, Guralnik JM, Haskell W, Lovato LC, Pahor M, Pepine CJ, Reid KF, Newman A. Ankle brachial index values, leg symptoms, and functional performance among community-dwelling older men and women in the lifestyle interventions and independence for elders study. J Am Heart Assoc. 2013 Nov 12;2(6):e000257. doi: 10.1161/JAHA.113.000257. PMID: 24222666; PMCID: PMC3886743.
[ii] McDermott MM, Greenland P, Liu K, Criqui MH, Guralnik JM, Celic L, Chan C. Sex differences in peripheral arterial disease: leg symptoms and physical functioning. J Am Geriatr Soc. 2003 Feb;51(2):222-8. doi: 10.1046/j.1532-5415.2003.51061.x. PMID: 12558719.
[iii] The Natural History of Intermittent Claudication, Kewwani, Amit N., MD and Beckman, Joshua A., MD., Endovascular Today, September 2019
[iv] Harada, M., Matsuzawa, R., Aoyama, N. et al. Asymptomatic peripheral artery disease and mortality in patients on hemodialysis. Ren Replace Ther 4, 17 (2018). https://doi.org/10.1186/s41100-018-0159-6.
[v] Current accepted hemodynamic criteria for critical limb ischemia do not accurately stratify patients at high risk for limb loss, Vallabhaneni, Raghuveer et al., Journal of Vascular Surgery, Volume 63, Issue 1, 105 – 113.